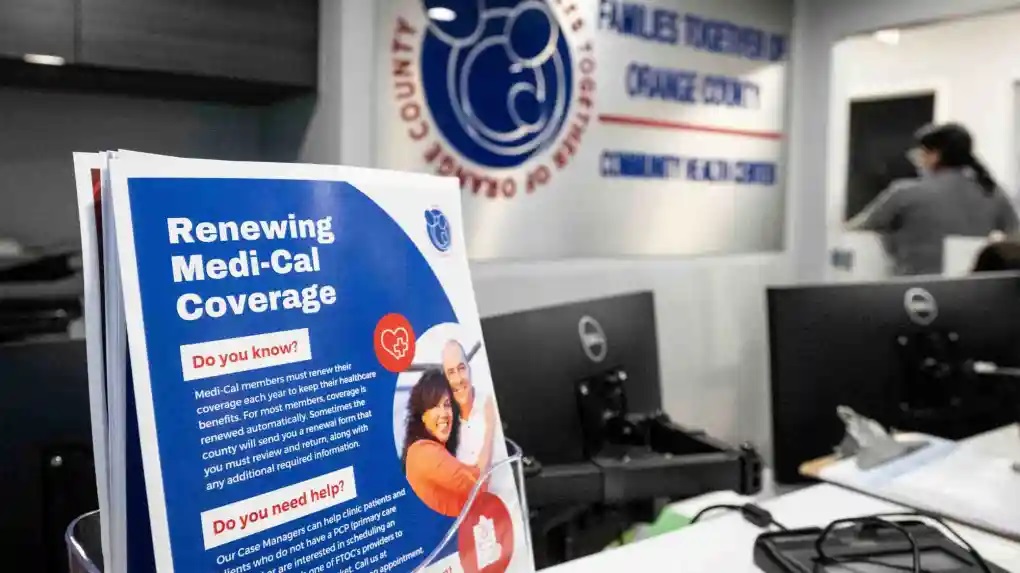
More than 700,000 immigrants ages 26-49 are expected to qualify for full health insurance come Jan. 1 when California takes the final step in opening up Medi-Cal, the state’s health care program for low-income residents, to everyone who meets eligibility requirements, regardless of their immigration status. (Photo by Paul Bersebach, Orange County Register/SCNG)
California legislators want the state to provide free health care to every resident, including undocumented immigrants.
Assembly Bill 2200 would make CalCare the state’s single-payer health-coverage provider. Under the act it would be illegal for any resident to pay a doctor privately for any medical treatment covered by CalCare.
To accomplish this goal, the legislators hope to convince the federal government to turn over all California Medicare funding so they can force every senior into the new system. Ditto for Medicaid. Employer-provided health insurance would also vanish. Instead of paying premiums and medical bills for private coverage, employers and their employees would have to pay taxes to CalCare
More taxes. Even if the federal government forced Medicare beneficiaries into CalCare, and CalCare collected all Medicaid and employer insurance payments, it would still need additional revenues to replace out-of-pocket spending by individuals.
In 2023 a bill to fund California single-payer care, ACA 11, was tabled. It would have imposed higher individual payroll taxes, higher income-tax rates with a top marginal tax rate of 18.05 percent, and taxes on gross business revenues. The Tax Foundation estimated it would increase taxes by $12,250 per household, doubling the current tax burden.
“Medicaid for all.” If everyone had to be in the same health plan, what would the system look like? Almost certainly it would spur a race to the bottom.
Wherever we look in the world, we find that government-run health care tries to control costs by squeezing the providers. In California, that would mean paying doctors and hospitals Medicaid rates – or perhaps even less.
According to Urban Institute researchers, California’s average Medicaid payments to providers are already significantly lower than in other states, amounting to about three-quarters of Medicare’s average payments.
And Medicare pays physicians and hospitals less than cost. Hospitals lost 12 percent on Medicare inpatients in 2022. Private payers currently pay 143 percent of Medicare rates for physician services and 189 percent for inpatient hospital care.
In 2017 only 48 percent of private California physicians accepted new Medicaid patients, so they wait months or years for appointments. Under CalCare, everyone would be waiting.
Rationing by waiting. During the COVID-19 pandemic, California met the surge in medical needs by paying traveling nurses as much as $5,000 a week to attract them from out of state. Under CalCare no hospital could afford to do that. On the contrary, doctors and nurses would leave the state seeking better pay (and lower taxes).
What would happen when demand for care surged (because it was free) and supply shrank (as the providers left for greener pastures)? The answer has almost always been: rationing by waiting.
According to the 2023 edition of the Fraser Institute’s Waiting Your Turn, Canadians on average wait more than 6 months from referral by a general practitioner to treatment by a specialist. Patients, including women showing symptoms of breast cancer, wait more than three months for an MRI scan.
Unable to get the primary care that Americans expect, Canadians frequently turn to overcrowded emergency rooms, where some die waiting for hospital beds.
England’s National Health Service (NHS) staffing and bed shortages are so bad that almost 14 percent of planned hospital surgeries are canceled on the day scheduled. Ten percent of canceled patients had suffered previous cancellations. Recently, a woman with a severe skin condition waited four years to see a dermatologist.
Covering up failure. Governments rarely like to admit their mistakes. Over 20 years of structural failures in NHS maternity centers injured or killed thousands of babies. Those infant deaths were hidden by the bureaucracy. Each scandal uncovered since the 2015 Morecambe Bay report has been investigated. Reforms have been announced, but the systemic failures remain.
In the United States, Veterans Administration (VA) officials were caught covering up failure by falsifying waiting–list datain 2014. They were forced to reduce wait lists by paying for private care. Subsequent comparisons of VA and private surgical outcomes found no adverse quality differences as a result of using private services to obtain prompt care.
No exit. Eliminating private payment for covered services is such a bad idea that even Canada has given up on it. Canadians who had been enduring up to two years of pain waiting for hip surgery can now pay privately and wait only two months.
Bad as you may think California health care is now, passing CalCare will make it much, much worse.
Read the original article on the Orange County Register website.
0 Comments